Blood Testing 101
When taking hormone replacement therapy (HRT), keeping tabs on your health is crucial. Regular blood testing can help you ensure your hormone levels are where they need to be and helps monitor for any side effects. Here's a beginner-friendly guide to blood testing as a trans person.
Why Test Blood?
Blood tests are essential for safe and effective HRT, serving two main purposes:
Dose Adjustments
The body's response to HRT varies from person to person. Blood tests can help you fine-tune your HRT dosage for your unique body. If your hormone levels are too low, this can mean that you might not be getting the changes you want. If your hormone levels are too high, this can put you at increased risks of adverse side effects such as blood clots and liver problems.
Dose Adjustments
HRT can sometimes come with some side effects. Regular testing can help catch any issues early.
The main side effects of HRT are:
- Increased risk of blood clots in trans people taking oestrogen [1, 2]
- Increased risk of liver problems (especially in trans people taking testosterone blockers) [1, 2]
- Increased risk of polycythaemia (too many red blood cells in your body which can lead to stroke, only in trans people taking testosterone) [1, 3]
- Increased risk of low bone density (only in trans people using hormone blockers without also taking testosterone or oestrogen)
- Increased risk of breast cancer (only in trans people taking oestrogen - so learn to check your chest) [1, 2]
- Increased risk of having high prolactin levels (only in trans people taking oestrogen) [1, 2]
- Potentially increased risk of heart disease [1, 2]
- Potentially increased risk of diabetes [1]
- Fertility loss [1, 2, 3]
What Tests Do I Need?
Before Starting HRT
Many clinical guidelines recommend doing blood tests before starting HRT. These tests provide a reference point (often called a baseline) for tracking changes in your hormone levels. They also allow you to spot any health conditions you might already have. If new symptoms or health issues pop up later, having this initial data makes it easier to figure out whether they are related to HRT or another cause.
Some baseline tests that may be useful are:
- Hormone levels: testosterone (T), oestradiol (E2), follicle stimulating hormone (FSH) and luteinising hormone (LH) [2, 3]
- Prolactin (PRL) [2, 3]
- Vitamin D [2, 3]
- Sex hormone binding globulin (SHBG) [2, 3]
- Liver function tests (LFT) [2, 3]
- Urea and electrolytes (U&E) [2]
- Fasting lipids (this test should be done after 12 hours of fasting) [2, 3]
- HbA1c to check your diabetes risk [2, 3]
- Haemoglobin (Hb) or haematocrit (Hct) [1, 3]
Monitoring Tesosterone Replacement Therapy
For people taking testosterone:
- Testosterone (T) and oestradiol (E2) [1, 3]
- Haemoglobin (Hb) or haematocrit (Hct) [1, 3]
- Liver function tests (LFT) [3]
- Fasting lipids [1, 3]
Monitoring Oestrogen Replacement Therapy
For people taking oestrogen:
- Testosterone (T) and oestradiol (E2) [1, 2]
- Prolactin (PRL) [1, 2]
- Liver function tests (LFT) [2]
- Progesterone (if you are taking progesterone)
How To Do Blood Testing
How Frequently Should I Test?
It takes time for your body to adjust to HRT, so blood tests won't immediately reflect dose changes. As such, many guidelines suggest testing every 3 months during your first year on HRT and every 6-12 months after that [1, 2, 3].
When Should I Take My Test?
Your hormone levels on HRT vary depending on when and how you take your medication. Some forms of HRT, like tablets and gels, are absorbed into your blood quickly and reach peak levels within hours. Other forms of HRT, such as injections, can take days to peak and then gradually decline. Blood tests taken at the right time give the most useful results to help fine-tune your HRT dosage.
Typical timings for common forms of HRT are:
- Injections:
- At trough (lowest level - just before the next injection) for the first test [1, 3]
- At peak (highest level - timing depends on injection type) for the second test [1, 3]
- Gels: 4-6 hours after application [2]
- Patches: 24-72 hours after application [2]
- Tablets: 4-6 hours after taking the tablet [2]
Convenient At-Home Testing
At Sapphic Bison, we offer an at-home blood testing service designed specifically for transgender people in the UK. Our service is not-for-profit, making it a convenient and affordable way for many people on HRT to monitor their health.
That said, our tests are not suitable for everyone. You should consider another testing method if:
- You have a blood clotting disorder
- You have very poor blood circulation in your hands
- You are doing HRT with gels
Our tests use kits that are posted to your home. Each kit contains a small blood collection tube and lancets (tiny medical devices with a sharp point that are used to prick your finger). You use the lancet to make a small puncture in your skin, allowing a few drops of blood to collect in the tube. Once your sample is ready, you post it back to us using the prepaid packaging.
We work with partner laboratories to analyse blood samples. All our partner laboratories are UKAS accredited which means that they carry out regular validation work to ensure that at-home blood samples provide results comparable to those from venous samples. There are also several peer-reviewed scientific papers that show that at-home tests match the accuracy of venous tests for hormones and liver health [4, 5].
Tips for Getting the Best Sample
If you haven't completed an at-home test before (or have previously had difficulty collecting enough blood), you might find these tips useful:
- Carefully follow the instructions that come with the test kit
- Keep your hand below heart level (e.g. by standing up, or by placing the collection tube on a low surface)
- Drink plenty of water and do gentle exercise (e.g. walking or stretching) just before you collect your sample to improve blood flow
- Wash hands with warm water to increase blood circulation to your hands
- If you're struggling to get enough blood, try holding a cup of a warm drink for a minute to warm your fingers
- Get a trusted friend or healthcare professional to help you (this can be especially helpful if this is your first time)
You can watch this video for a visual demonstration on how to take the test.
Once you've collected your sample, post your test kit as soon as possible - ideally on the same day, before the last collection time in your area. You can find your nearest post box and its last collection time by visiting the Royal Mail website.
What Can Go Wrong?
There are a few things that can go wrong or lead or an error in your test results. Here's how you can avoid them:
- Haemolysis (damage to the red blood cells in the sample which can cause inaccurate results)
- Avoid squeezing your finger too hard when collecting the sample
- Avoid shaking the tube too hard after you've collected your sample
- Not enough blood collected
- Try using the tips above to help improve circulation and blood flow
- Phobia of needles
- Try using these tips from the NHS for overcoming needle phobia
- Ask a friend or nurse for assistance
- Clotting of the sample
- Make sure to wipe away the first drop of blood after pricking your finger
- Contamination with gel
- Avoid using a capillary test if using gels as contamination causes inaccurately high results
I Have Results, Now What?
Understanding Your Results Sheet
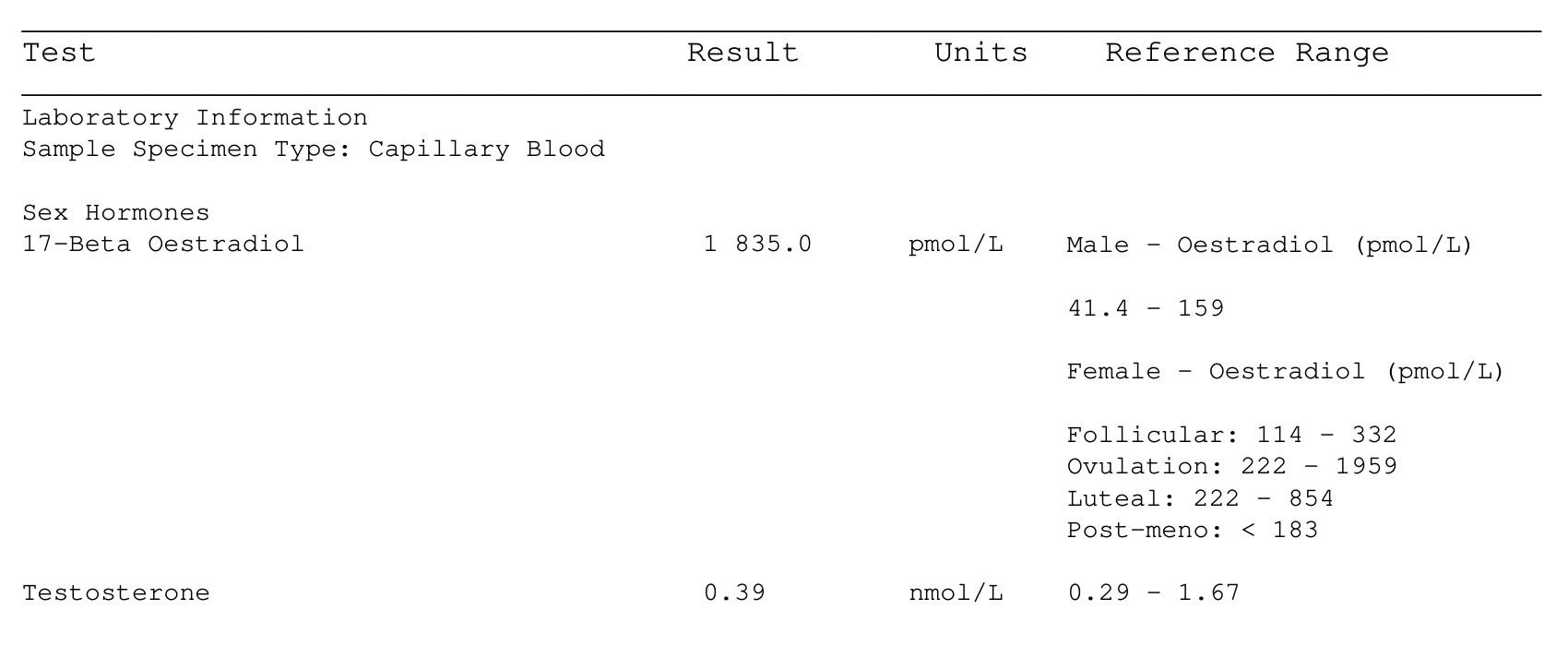
Your lab results sheet might look like this:
Let's break it down.
- The first column (Test) lists each test your sample took. Your results might also include other tests such as liver function or blood count.
- The second column (Results) shows you your result for each individual test.
- The third column (Reference Range) shows the range of results that are considered “normal” (more on this later).
- The fourth column (Units) shows the measurement unit for each result. It is important to note that different laboratories might use different units to measure the same thing. For example, while we report oestradiol in pmol/L (picomoles per litre), other labs might use units such as pg/mL (picograms per milliliter).
Reference Ranges
You can check whether your results are “normal” by checking each one against its corresponding reference range.
Reference ranges are based on scientific studies and represent the values found in 95% of the population. They provide an expected range for each result, from the lowest to the highest value. Some reference ranges come with extra information, notably oestradiol. The “female” reference range for oestradiol is often divided into four categories: follicular, ovulation, luteal and post-menopause. The first three correspond to the different parts of the menstrual cycle. This can be confusing, but for trans people on oestrogen, most medical guidelines suggest staying below the peak levels seen during ovulation to ensure safe and effective treatment [1, 2].
It is important to mention that some test results may be abnormal due to reasons other than HRT. For example, while too much prolactin can sometimes be caused by tumours, it can also be caused by use of antidepressants or antipsychotics, or simply by nipple stimulation. You should be careful when noting your results but don't get too anxious if your results are slightly outside the ranges. This also highlights the importance of measuring baselines to know if your levels were changed after HRT.
Where to Go If We Can't Help You
- Your GP
- Consider reacing out to Spectra's trans healthcare advocacy services if you have issues consulting with your current GP due to discrimination or other related issues
- If you are forced to change GP due to discrimination, you might find Trans Healthcare Intelligence's list of trans-friendly GPs helpful.
- CliniQ in London
- 56 Dean St. in London
- Other suppliers who offer nurses and venous blood tests (e.g. Randox)
Sources
This explainer was written in consultation with clinicians. We also used several clinical and scientific sources.
- Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2017;102(11):3869-903. [Link]
- Seal L, Barrett J. Shared Care Prescribing Guidance for the Treatment of Gender Dysphoria in People Assigned Female at Birth Transitioning to a Masculine Gender Identity. Tavistock and Portman NHS Foundation Trust; 2024. [Link]
- Seal L, Barrett J. Shared Care Prescribing Guidance for the Treatment of Gender Dysphoria in People Assigned Male at Birth Transitioning to a Feminine Gender Identity. Tavistock and Portman NHS Foundation Trust; 2024. [Link]
- Vasavan T, Getreu N, Rutter E, Biggs R, et al. Capillary blood collection tubes containing serum separator gel result in lower measurements of oestradiol and total testosterone. Clin Chem Lab Med. 2023;62(4):e84-e86 [Link]
- Ansari S, Abdel-Malek M, Kenkre J, Choudhury SM, et al. The use of whole blood capillary samples to measure 15 analytes for a home-collect biochemistry service during the SARS-CoV-2 pandemic: A proposed model from North West London Pathology. Ann Clin Biochem. 2021;58(5):411-21. [Link]
Disclaimer
This explainer is for general informational purposes only and is not a subsitute for professional medical advice. Our full disclaimer can be read here.